Feeling at home
From bedside bingo to therapy dogs, we're here to help kids smile and feel more like themselves.
Visit Child Life services

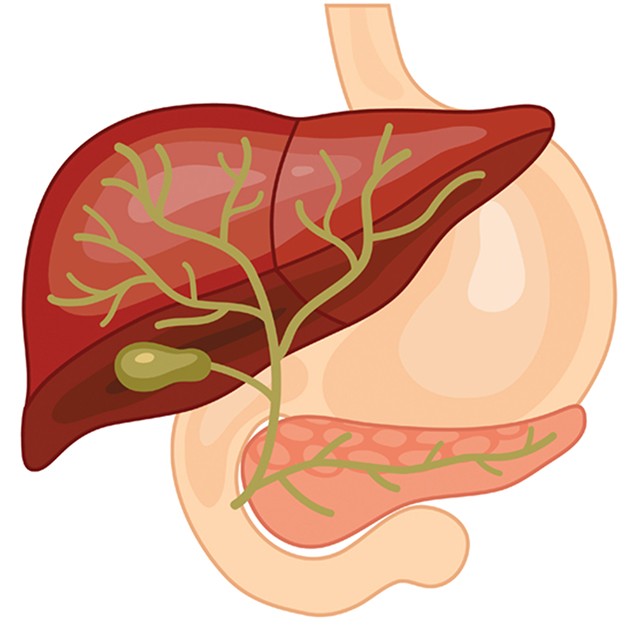
Primary sclerosing cholangitis (PSC) is a rare chronic disease that causes inflammation and scarring of the bile ducts. These are tubes that carry bile out of the liver (bile is a fluid that helps to break down fat in food). As scarring accumulates, the ducts become blocked, causing bile to build up in the liver and damage liver cells. If untreated, PSC can eventually cause liver failure or hardening of the liver, called cirrhosis. In either case, a liver transplant is needed.
We don't know why some children develop PSC, but research suggests it may be an autoimmune disease – a condition in which the immune system attacks healthy cells. Many children with PSC also have ulcerative colitis or, less often, Crohn's disease – autoimmune disorders that are both types of inflammatory bowel disease (IBD).
PSC affects boys more often than girls, and a family history of PSC or IBD increases a child's risk for developing the condition. We regularly screen children with IBD for signs of PSC so that we can start treatment promptly.
Children diagnosed with PSC need to be closely monitored, but with proper treatment, most can have a good quality of life.
UCSF's dedicated team of hepatologists (liver specialists) delivers cutting-edge, compassionate care for all kinds of liver disorders, including PSC. We monitor our PSC patients for any evolving problems related to the disease and address these issues proactively.
What's more, we are part of the Autoimmune Liver Disease Network for Kids (A-LiNK), a multicenter collaboration to improve the care and health of children and adolescents with PSC and other liver diseases.

Ranked among the nation's best in 10 specialties

Best in Northern California for gastroenterology & GI surgery
Symptoms of PSC are caused by poor drainage from the bile ducts. This can affect liver function and make bile seep into the bloodstream. In the early stages of PSC, your child may not experience any symptoms or may experience symptoms that come and go, such as:
As the condition progresses, symptoms of liver failure may develop, including:
A doctor's first steps in diagnosing PSC are to perform a physical exam and take a medical history. If these suggest your child may have PSC, various tests will be ordered, such as:
There is no established cure for PSC, but with close monitoring and symptom management, most kids with PSC can enjoy the normal activities of childhood.
Treatments include:
In severe cases, PSC leads to irreversible liver damage or failure. When this occurs, a liver transplant is needed. UCSF's Liver Transplant Program is known for outstanding outcomes and some of the best survival statistics in the country. Our program helped pioneer techniques that have made transplantation safer and more successful. For some patients, liver transplantation cures PSC.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
Advanced endoscopic procedures
A narrow tube with a tiny camera on the end provides a detailed view of the bile ducts and liver.
Liver transplantation through living donors
This lifesaving approach takes advantage of the liver's unique ability to regenerate.
Feeling at home
