Staff superheroes
It’s a bird. It’s a plane. It’s a window washer! Dressed as a superhero to clean and brighten your day.


Most cases of hepatitis are caused by viruses or exposure to toxins that damage the liver, but autoimmune hepatitis is a rare form that occurs when the body's immune system mistakenly attacks healthy liver cells. This assault inflames and damages the liver. If untreated, the disease can eventually lead to liver failure.
There are two types of autoimmune hepatitis, differentiated mainly by the presence of certain antibodies in the patient's blood. Type 1 affects people of all ages. Type 2 typically affects children; it tends to be more aggressive, and generally means patients have to stay on medication. Regardless of the type of autoimmune hepatitis your child has, the treatment is the same: medications that suppress the immune system.
We don't know why some children develop autoimmune hepatitis. Research suggests a possible genetic predisposition. The condition may also be related to underlying problems with the person's immune system or may be triggered by environmental factors, such as exposure to infectious agents, toxins or drugs.
As with most autoimmune diseases, this is a chronic condition. But with early intervention and close monitoring, it can be managed. Although there is no cure, most children respond well to treatment and some even achieve remission, allowing the liver to start healing and symptoms to go away.
UCSF Benioff Children's Hospitals offer the most advanced diagnostic and treatment options for children with autoimmune hepatitis, providing this care in facilities designed specifically for kids. Managing the disease through expert use of medications and close monitoring, we aim to reduce the risk of long-term liver damage. We're also part of the Autoimmune Liver Disease Network for Kids (A-LiNK), a multicenter collaboration working to improve the health of children and adolescents with autoimmune hepatitis and other liver disorders.
Ranked among the nation's best in 10 specialties

Best in Northern California for gastroenterology & GI surgery
Symptoms of autoimmune hepatitis depend on the severity of liver damage, but some of the more common include:
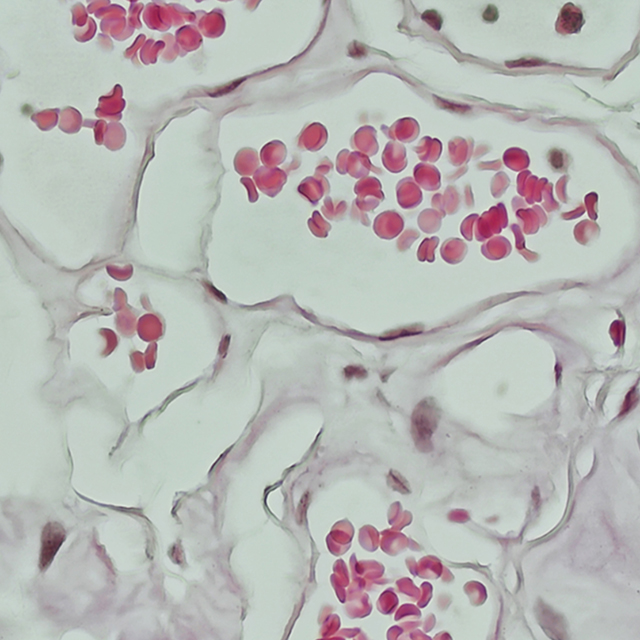
A doctor's first steps in evaluating your child will be to conduct a thorough physical exam and to take a medical history. To make a diagnosis, various tests are used, including:
The goals of treatment are to suppress the overactive immune response and to prevent further liver damage. We mainly use two types of medication:
We monitor patients closely with regular lab tests, ultrasounds or other imaging tests, and clinic visits. In some patients, the disease goes into remission, meaning there are no symptoms or signs of ongoing liver damage.
If your child's blood work is completely normal for two years, we may be able to stop treatment. But before doing so, we'll need to perform a liver biopsy to confirm that there is no further liver inflammation. (It's possible to have normal blood work and persistent liver inflammation.) Even after active treatment ends, your child will need to be followed to make sure they don't relapse or develop other health issues.
If treatment isn't successful or the liver damage becomes severe, a liver transplant may be necessary. Our Liver Transplant Program, designated a center of excellence by the U.S. Department of Health and Human Services, is known for outstanding outcomes and for helping pioneer techniques that have made transplants safer and more successful. We perform more than 200 transplants each year and our survival statistics are among the best in the country.
UCSF Benioff Children's Hospitals medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your child's doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your child's provider.
Liver transplantation through living donors
This lifesaving approach takes advantage of the liver's unique ability to regenerate.
Staff superheroes
